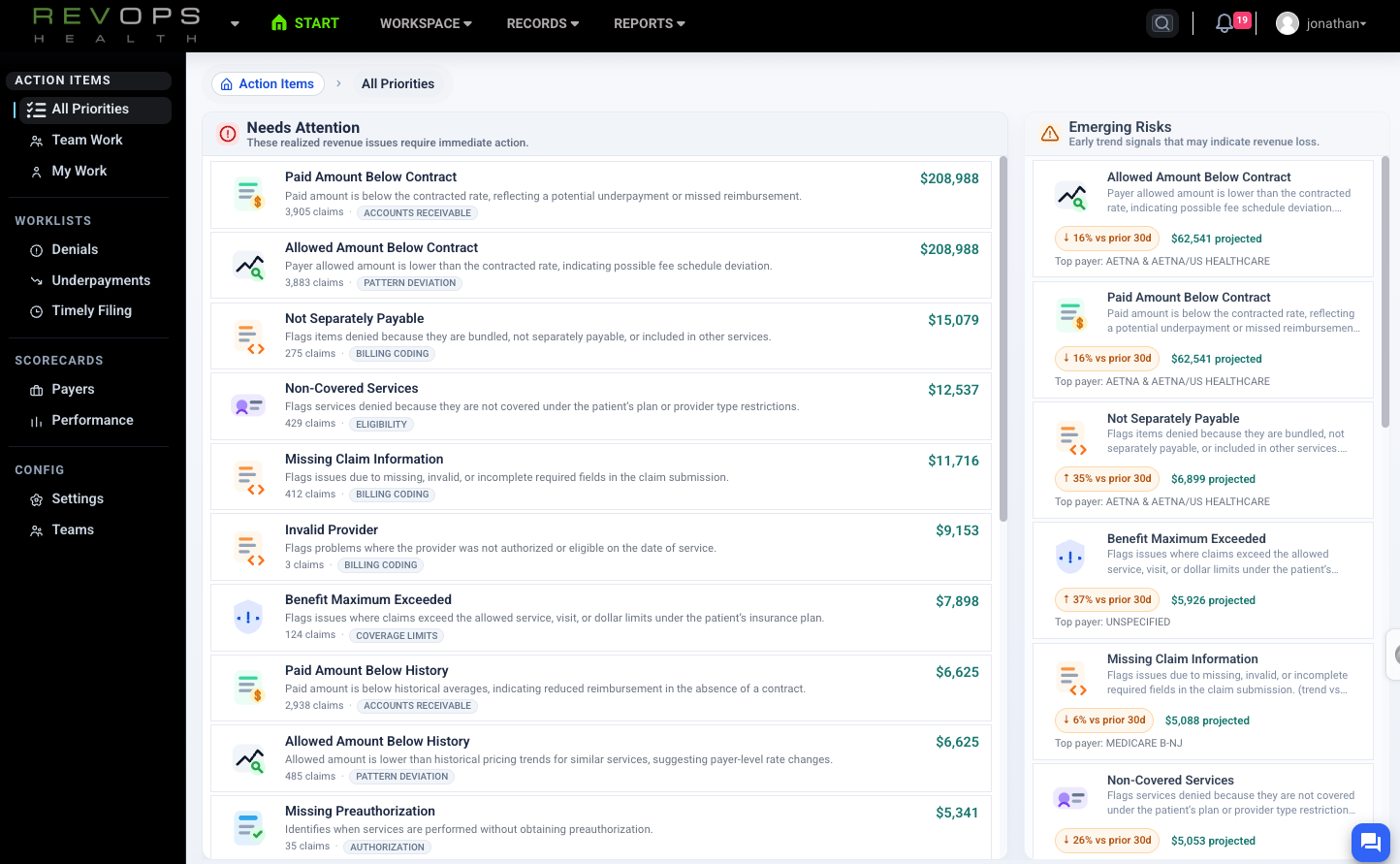
Get clean answers from messy revenue data
Analyze claims, payments, and payer behavior without wrestling spreadsheets or broken reports.
RevOps Health gives you a reliable, queryable view of claims and remittances so you can find issues, explain performance, and support decisions with confidence.
Trusted by independent clinics, provider groups, specialty practices, and small to mid size hospitals across the United States.
Why analysts use RevOps Health
As an analyst, you are expected to answer complex questions quickly.
Why revenue changed.
Which payer is driving variance.
Where money is leaking.
But data lives across systems, reports arrive late, and numbers do not always tie out.
RevOps Health gives you one source of truth you can trust.
What RevOps Health helps you do
Analyze without friction
Filter, segment, and drill into claims and payments without rebuilding reports or spreadsheets.
Trust the numbers
Work from clean, normalized data that reconciles across systems and holds up to scrutiny.
Explain performance
Tie trends to specific payers, codes, or workflows and answer questions in minutes instead of days.
How it works
Ingest and normalize
Claims and remittances are ingested and cleaned automatically.
Query and explore
Use filters, saved views, and comparisons to analyze performance.
Quantify impact
Every insight is tied to real dollar impact so findings are actionable.
Analyst / Power User FAQs
-
Traditional BI tools are brittle, static, and dependent on periodic data pushes. RevOps is a search-based analytics platform that rebuilds your data nightly, allowing you to ask new questions of fresh data instead of forcing questions into prebuilt reports. Views are flexible, dynamic, and designed to evolve with how you analyze.
-
Yes. Every chart in RevOps is backed by underlying data that’s accessible in a few clicks. You can drill from trends to claim-level detail, view all related claims, remittances, patient payments, and write-offs for an encounter, and export everything instantly for further analysis.
-
RevOps uses indexed search “chips” that let you filter across ranges, categories, and tagged states like unpaid, partially paid, or fully paid. As data is processed, it’s enriched with contextual signals, allowing you to query your RCM the way you’d query Google—by intent, not report structure.
-
Absolutely. RevOps allows you to analyze across payers, service lines, locations, provider groups, time periods, and more. Built-in comparison tools support side-by-side analysis, making it easy to identify outliers, trends, and performance gaps across the organization.
-
Edge cases are addressed continuously by our engineering team as they’re identified. Payer logic ultimately resolves into standardized claim and remittance structures (837s and 835s), which RevOps fully parses and analyzes. For Pro and Max tiers, we layer in PM system signals to add practice-specific context.
-
Clearinghouse and PM analytics reflect only their narrow view of the workflow—often focused on claim submission success, not payment accuracy. RevOps analyzes outcomes contextually, identifying anomalous behavior, underpayments, delays, and inconsistencies across similar claims. Think spellcheck versus grammar check.
Spend less time fixing data
Spend more time answering the questions that matter.